Most of our lives we are caught up in the moment. Let’s now take a moment to look at diabetes
from 10,000 feet up, where we can see clear patterns and insight emerge from
the fog of hypoglycemia, and its opposite, hyperglycemia. If we plot
carbohydrate consumption
from low to high on the y-axis, and injected, fast acting (bolus) insulin from low to
high on the x-axis, we can see all possible combinations of expected results on
the following matrix:
When injected bolus insulin is low or zero,
and carbohydrate consumption is
high, we are presented with the classical triad of diabetes symptoms: polyuria, polydipsia, and polyphagia: respectively, frequent
urination, increased thirst and consequent increased fluid intake, and
increased appetite. Other manifestations
will include weight loss (despite normal or increased eating), irreducible
fatigue, and changes in the shape of the lenses of the eyes,
resulting in vision changes.
When the glucose concentration in the blood is raised beyond the
renal threshold, reabsorption of glucose in the proximal renal tubuli is incomplete,
and part of the glucose remains in the
urine, which is called glycosuria.
Patients may also present with
diabetic ketoacidosis (DKA), an extreme state of metabolic dysregulation
characterized by the smell of acetone on the patient's breath; a rapid, deep
breathing known as Kussmaul breathing; nausea; vomiting and abdominal pain; and
any of many altered states of consciousness or arousal (such as hostility and
mania or, equally, confusion and lethargy).
In severe DKA, coma may follow, progressing to death.
Surrounding this cell on the
matrix is hyperglycemia, both to the right, when
carbohydrates consumed are high and injected insulin is moderate, but
not enough to cover the load, and below, when a decrease in carbohydrates is
consumed, but still not offset enough by injected insulin.
In the middle of the chart, where
one eats a moderate amount of carbohydrates and injects a moderate amount of
bolus insulin, lies the typical diabetes treatment. “Eat a balanced diet and learn to adjust your
insulin accordingly” is
the principal treatment that is followed here.
It is possible to attain near-normal A1c levels with this approach,
however, normal levels of cholesterol, weight, and blood pressure may prove unreachable.
Furthermore, this area of the
table is fraught with negative consequences at nearly all adjacent and opposite
borders. Not enough insulin puts one in
hyperglycemia territory both to the left and above. Not enough carbohydrates, and one finds
themselves hypoglycemic to the right and below.
At the other extreme, when
injected insulin is high, and
carbohydrates consumed are too low, severe hypoglycemia could result,
necessitating a visit from the local paramedics when subsequent low blood
glucose causes
unconsciousness. If not attended to
quickly, coma and death could occur within minutes.
Too, if carbohydrates and insulin injected are high,
the result is a hyper-hypo-glycemic swing—a rollercoaster ride if you will—of
great magnitude, where the patient is constantly adjusting carbohydrate and insulin loads to offset
their blood sugar.
But look what happens when both
carbohydrates consumed and insulin injected are as
low as possible. At the far lower-left
cell of the matrix, one doesn’t eat a great many carbohydrates, and,
subsequently, does not need to inject much insulin as a result. In this case, one can achieve a stable and
normal blood sugar concentration, and enjoy the benefits of a normal life:
lower VLDLs, higher HDLs, stable or decreasing weight, and less anxiety not
having to think about whether one has injected the right amount of insulin. And testing can
be reduced to once a day, in the morning, to validate your successful Insulin
Glargine dosing, i.e., whether or not your morning BG
is in the 70-110 mg/dL range. This home
base is where thriving begins.
At the zero bolus-insulin and near-zero
carbohydrate home, you may thrive for a long, long time. There
are three major centenarian studies going on around
the world, the New England Centenarian
Study, the Georgia Centenarian Study and the Okinawa Centenarian Study. According
to Dr. Ron Rosedale:
They are trying to find the
variable that would confer longevity among this group of people who live to be
100 years old. Why do centenarians become
centenarians? Why are they so
lucky? Is it because they have low
cholesterol, exercise a lot and live a healthy, clean life?
What researchers are finding
from these major centenarian studies is that there
is hardly anything in common among these people. They have high cholesterol and low
cholesterol, some exercise and some don't, some smoke, some don't. Some are nasty as can be, some nice and calm
and some are ornery. But, they all have
relatively low sugar for their age, and they all have low triglycerides for
their age. And, they all have relatively
low insulin…The way to treat virtually all of the so-called
chronic diseases of aging is to treat insulin itself” (“Insulin and its
Metabolic Effects,” Ron Rosedale,
Signs for Health Institute’s BoulderFest, August, 1999).
Although the use of exogenous
bolus insulin as a treatment to
mitigate the effects of carbohydrate consumption was innovative, exciting, and
promising nearly a century ago, its use has become—save on the acutely serious
hyperglycemic—obsolete with the introduction of Insulin Glargine, and the knowledge that carbohydrates are non-essential.
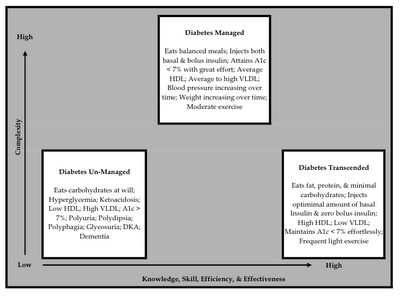
A remarkable picture develops when you take those
three highlighted cells from the previous figure and place them on two
different axes, one a continuum of complexity from low to high, and the other,
a continuum of knowledge, skill, efficiency, and effectiveness, again, from low
to high.
The y-axis, complexity, relates to the treatment—medication &
nutrition—and lifestyle a person implements or recommends. Regarding the x-axis, knowledge, skill,
efficiency, and effectiveness, it could be looked at from two perspectives;
one, from a diabetic’s perspective, where the focus is on their knowledge &
skill as it relates to implementing advice from a third-party or self-directed
behavior, and another, from the perspective of a third-party’s knowledge &
skill, be it friend, relative, caregiver, nutritionist, nurse, or doctor. Treatment efficiency and effectiveness in
either case is also measured.
The lowest complexity matched with the lowest skill & knowledge,
will result in a diabetic on the brink.
It is quite easy for them to eat carbohydrates at will and develop the
hyperglycemic symptoms of full-blown diabetes: polyuria, glycosuria, polydipsia, polyphagia, ketoacidosis, weight loss, etc., culminating in shortened life
span. Knowledge for the patient about
diabetes may be non-existent, and they will likely seek out medical attention
for help, though, unfortunately, some don’t or for many reasons even if they
do, helpful advice is not available.
Acquaintances will also most likely notice the change in persona or
appearance, and they too will make it a point to tell the person that something
is wrong.
“Diabetes Managed” represents a diabetic trying to follow the
instructions and advice of his or her general practitioner, though both are
influenced by a wide variety of stakeholders with oftentimes divergent
self-interests. A majority of the
influencers in the medical advice providing supply chain include:
·
Pharmaceutical
companies
·
Researchers
·
Doctors
·
Endocrinologists
·
Nutritionists
·
Educators
·
American Diabetes
Association
·
World Health
Organization
·
Medical schools
·
Nurses
·
Reference media
such as the Physician’s Desk Reference
·
Food
manufacturers
·
Food marketers
·
Popular internet
sites, print media & the news
·
Friends, family,
co-workers & acquaintances
By default, advocates of each group act in their own perceived best
interest, based upon their knowledge and skill, which may in turn be based upon
the state of information available at their time of training or education. Many of the above stakeholders, with the
exception of the end users themselves—the people with diabetes—have significant
power. In fact, some have a near-absolute
advantage in the marketplace—the ability to influence behavior without question
or pause—leaving the buyer of an optimal diabetes treatment treating their
diabetes sub-optimally, i.e., carbohydrate &
bolus-insulin intensive.
And the results? Perhaps an HbA1c at or below 7%,
weight gain, increasing VLDL levels,
increasing blood pressure, too much time spent counting carbohydrates and
measuring insulin doses, anxiety
caused by constantly wondering whether or not too much or too little
carbohydrates were eaten or insulin dosed, the ever
present chance of hypo- or hyper-glycemia, constant blood sugar testing, and
the list goes on. “Diabetes Managed” may
not achieve optimal results for the end user, but, for the other stakeholders,
it brings and keeps customers longer.
Although the science behind the drugs that either limit the amount of
glycogen released from the liver or that bind
and carry glucose from the blood
to the receptors that transport it across cell membranes is remarkable, it is
based upon two assumptions: (I) that carbohydrates are an essential majority
part of the diet, and/or (II) that through education, a patient cannot, will
not, or should not keep from consuming them.
Remove those key assumptions, and the house of cards from which that
remarkable science is based comes toppling down.
Caveat emptor. “Diabetes
Managed” may be the first natural step for diabetics to enter—a complex
medical-advice-providing system—in progression of their self-treatment, but it
doesn’t have to be.
As knowledge about diabetes increases, trusted advisers and patients
alike will choose a less-complex method, one that transcends diabetes by avoiding
the root cause of symptoms and complications—carbohydrates—and replacing those
carbohydrates in the diet with fat, resulting in benefits such as healthy
weight loss, lowered VLDL levels,
increasing HDL levels, reduced
mTOR activity,
normal blood pressure, etc.; in short, leading to a longer, happier, healthier
life.
To transcend diabetes requires reduced carbohydrate consumption to
near zero, with emphasis on a combination of fats and
protein. It is orders
of magnitude less complex, less worrisome, and less risky than counting
carbohydrates and matching it with doses of insulin. It is simple.

This comment has been removed by a blog administrator.
ReplyDelete