“No one in this world, so far
as I know, has ever lost money by underestimating the intelligence of the great
masses of the plain people.” H.L.
MENCKEN, Chicago Tribune, September 19, 1926
The following article was
originally a chapter in my second book, ESSENTIAL DIABETES LEADERSHIP (2010). I still wonder whether or not I am making a
mountain out of a molehill of it and whether the reaction to my definitely
inelegant tables would be: “True; but, of course, all fairly obvious.” As to the making of the mountain, if such it is,
I am utterly tired of it and prefer to write novels. Nonetheless, my increasing confidence in the
basic application of low-, very low-, or near-zero-carbohydrate diets as a
template for health—so many people are healthier for it—decided me that I’m
probably not a crank.
It is hard even to feel and
harder still to write in a way that runs counter to a current world view,
especially a moral one, and it is all the harder when the way is re-shaping a
plane of perfection to which all civilized cultures are thought to be striving. A scientist or philosopher with a program of
such heresy has to be tough if he or she is to communicate it and, while doing
so and for long after, must endure the tortures of Orestes.
I do so love repurposing the
elegant words of those I hold in high esteem and if you now think “kinship
selection” and “evolution” instead of “low-carbohydrate diet” you will recognize
that the above words were written by W.D. Hamilton and were sourced from
several articles comprising NARROW ROADS OF GENE LAND. They convey my feelings well, and, with them,
I introduce you to my “Dilemmas.” Best wishes…
- lc
This book [ESSENTIAL DIABETES
LEADERSHIP] was written in the conviction that an optimal solution to diabetes
once presented a great mystery, but that it is a mystery no longer because it
is solved.[1] Dr. Richard Bernstein solved the problem by experimenting with his
diet, notably by reducing his consumption of carbohydrates. In so doing, Dr. Bernstein validated the work
done nearly a century before him by Richard Thomas Williamson, Charles Purdy,
and many others, who, of course, validated John Rollo’s solution recommended
100 years before them. We have added,
and shall continue to add, footnotes to the optimal solution, such as developing
the insulins glargine & detemir that enable us type 1s to achieve a normal,
stable blood sugar level in our sleep, upon awakening, and throughout the day.
Too, I wrote this book because I continue to be surprised and dismayed that
so many people seem not only unaware of the elegant and beautiful dietary
solution to our problem; but, incredibly, actually many are unaware what the
problem is in the first place!
There are two problems, really.
First, diabetes mellitus manifests
itself in our bodies as ineffective carbohydrate processing due to an insulin
function disturbance; we produce too much, too little, or none at all. And second, the optimal solution espoused
by would-be health-providers may be optimal for their needs, not ours. Humbly, though passionately, I hope that my
books—and the citations therein—have removed all sane doubt as to the veracity
of the first problem and its solution.
Explaining, proving then solving the second problem is the focus of this
chapter.
So to present this material, let me briefly
introduce an effective framework for understanding relationships between people
with opposing interests, the basis of all dilemmas. We will then apply this device to a couple of
real-world scenarios. “Game theory” is
thus our topic, William Poundstone our teacher, PRISONER’S DILEMMA our
textbook, and the decision strategy of a couple of imprisoned gang members our
subject.
Two members of a criminal
gang are arrested and imprisoned. Each
prisoner is in solitary confinement with no means of speaking to or exchanging
messages with the other. The police
admit they don’t have enough evidence to convict the pair on the principal
charge. They plan to sentence both to a
year in prison on a lesser charge.
Simultaneously, the police offer each prisoner a Faustian bargain. If he testifies against his partner, he will
go free while the partner will get three years in prison on the main
charge. Oh, yes, there is a catch. If both prisoners testify against each other,
both will be sentenced to two years in jail.[2]
The prisoners are given
little time to think this over, but in no case may either learn what the other
has decided until he has irrevocably made his decision. Each is informed that the other prisoner is
being offered the very same deal. Each
prisoner is concerned only with his own welfare—with minimizing his own prison
sentence. The below 2x2 matrix
graphically depicts the scenario. Note
that the first number in each cell is the payoff in terms of jail time for the
row player, “A,” and the second number in each cell is the payoff in terms of
jail time for the column player, “B.”
The prisoners can reason as
follows: “Suppose I testify and the other prisoner doesn’t. Then I get off scot-free, rather than
spending a year in jail. Suppose I
testify and the other prisoner does too.
Then I get two years, rather than three.
Either way I’m better off turning state’s evidence. Testifying takes a year off my sentence, no
matter what the other guy does.”
The trouble is, the other
prisoner can and will come to the very same conclusion. If both parties are rational, both will
testify and both will get two years in jail.
If only they had both refused to testify, they would have got just a
year each!
And so ends this short but
prophetic tale. For a great primer on
game theory, you are encouraged to read William Poundstone’s classic book PRISONER’S
DILEMMA: JOHN VON NEUMANN, GAME THEORY, AND THE PUZZLE OF THE BOMB (New York:
Doubleday, 1992). Here we will move from
theoretical games to the actual challenge, for that is where we—fellow members
of the club—find ourselves.
You go to your
health-provider(s) with the classical triad of symptoms of polyuria,
polydipsia, and polyphagia—respectively, frequent urination, increased thirst and
consequent increased fluid intake, and increased appetite—with the hope that they are more knowledgeable than
you and will help you find an optimal solution.
But therein lies the dilemma: your health-provider(s) may not be fully
vested in your interests alone.
Much has been written on the
subject. In “Conflict of Interest in
Clinical Practice,” (2007), first published in Chest, the author Mark R.
Tonelli, M.D., M.A., FCCP, provides some background:
“The inherent tension built into remuneration for the healing arts has been
recognized as far back as Plato, who devoted a small part of The Republic[3]
to the issue.[4] In a classic fee-for-service arrangement,
physicians benefit financially from the provision of more interventions, with
patients and the market poorly positioned to make judgments regarding the
necessity of these services.[5] Historically, a physician’s service largely
equated with the physician’s presence, but systemic conflicts of interest could
still arise, such as agreements for fee splitting from referrals or commissions
from pharmacies. As the number and kinds of medical services have exploded over
the last half-century, so has the potential for clinicians to profit from the
profligate use of these services. The
practice of medicine now provides the entrepreneurial physician with ample
opportunities to develop ancillary business interests, such as owning radiology
and other diagnostic or therapeutic centers or equipment, even entire
hospitals.[6] Clearly, the attendant financial gain in
“self-referring” a patient for testing or intervention under such circumstances
creates a conflict of interest as, logically, only a subset of patients will be
likely to benefit from the additional procedures, whereas all patients (at
least all those with the ability to pay) sent for testing or intervention would
financially benefit the physician-owner.
Empiric evidence amply demonstrates that such circumstances lead not
simply to a perceived conflict of interest, but to a marked increase in
utilization of services when compared to financially disinterested clinicians.[7],[8]
We’re primarily concerned with the ongoing treatment of diabetes, so,
admittedly, there’s little to worry that your general practitioner will
recommend visiting a radiologist in exchange for a small referral fee when
presented with your potential blood sugar surges. There are, however, other ancillary service
providers in the supply chain that would be happy to pay a small referral fee
for a new customer, e.g., an endocrinologist, dietician, exercise trainer,
laboratory technician. The predominant
source of referrals, better stated, gifts, as the authors of the article
suggest, are the pharmaceutical and medical device providers.
“Over the last several years,
particular professional and public attention has been focused on conflicts of
interest that arise from various relationships between the pharmaceutical and
medical device industries and clinicians.[9] Businesses that happen to make drugs or
medical devices have interests that are no different than those of other
businesses: maximizing shareholder value, generally by increasing sales.[10] The profession of medicine, in general, and
individual practitioners, in particular, continue to embrace a primary goal of
improving and maintaining the health and well-being of individual
patients. A conflict of interest
develops when interactions with industry create circumstances in which the
individual physician’s interest coincides with that of business, not patients. Beyond appearances, such conflicts have demonstrated
the potential to alter physician practice in a manner that favors the
pharmaceutical industry at the expense of the patient. Multiple specific interactions between
industry and clinicians, including gift giving, consultancy arrangements,
support of CME and guideline development, create conflicts of interest that
vary in terms of effect, but each acts to bias the clinician away from patients
and toward the interests of industry.”[11],[12]
And, in case you wondering
about the percentage of doctors receiving these gifts, there was a study
performed recently that provides that information. In “A National Survey of Physician-Industry
Relationship,” (2007), the authors surveyed physicians to collect information
about their financial associations with industry and the factors that predict
those associations. They conducted a
national survey of 3,167 physicians in six specialties (anesthesiology,
cardiology, family practice, general surgery, internal medicine, and pediatrics)
in late 2003 and early 2004. The raw
response rate for this probability sample was 52%. Here are the results:
“Most physicians (94%)
reported some type of relationship with the pharmaceutical industry, and most
of these relationships involved receiving food in the workplace (83%) or receiving
drug samples (78%). More than one third
of the respondents (35%) received reimbursement for costs associated with
professional meetings or continuing medical education, and more than one
quarter (28%) received payments for consulting, giving lectures, or enrolling
patients in trials. Cardiologists were
more than twice as likely as family practitioners to receive payments. Family practitioners met more frequently with
industry representatives than did physicians in other specialties, and
physicians in solo, two-person, or group practices met more frequently with
industry representatives than did physicians practicing in hospitals and
clinics.”[13]
The results of this national
survey indicate that relationships between physicians and industry are common
and underscore the variation among such relationships according to specialty,
practice type, and professional activities.
And as you delve deeper into
the literature, specifically on the results of medical practice, the
information can leave you feeling quite pessimistic. According to Dr. Joseph Mercola, in his
popular natural health website:
“The traditional medical
paradigm contains fatal flaws that have led to this startling statistic:
doctors are the third leading cause of death in this country killing a quarter
million people a year. Cancer and heart
disease are the only two causes that have killed more people. Drugs, surgeries and hospitals are rarely the answer to chronic health
problems. Diet, exercise, and lifestyle
are the key components to staying healthy.”[14]
Hard to believe; but, if
there was nothing to the theory of good doctors doing what they were trained to
do with poor results, then surely if there were periods in recent memory
without available doctors, we would see sickness and/or death rates increasing. Alas, the evidence points in the opposite
direction. According to Barry Groves in
TRICK AND TREAT: HOW ‘HEALTHY EATING’ IS MAKING US ILL, Israel, Canada, the US,
and Columbia share a common occurrence:
“Doctors don’t often go on
strike, but it has happened sufficiently often for a disturbing trend to be
noticed. During the rare times that they
have gone on strike—in several countries—the death rate has always gone down.”[15]
Once again, you’re probably a
step ahead of this writing, so, yes, a read of DO WE STILL NEED DOCTORS by John
D. Lantos, MD, may be indicated here.[16] Although it is an interesting book, the
issues involved in the disintermediation of an entire channel from the
marketplace are a bit overwhelming, so I won’t discuss here whether or not we
need doctors other than to say that more likely than not—outside of acute
emergency medical situations, and to prescribe basal insulin and delivery
devices—as we will see, they probably need you more. The plain and simple fact is: we will see a
doctor.
Whatever it is that doctors
do—primarily consult with patients—potential customers have the perception that
doctors may provide hope; they know or can at least access information and
products that patients do not know or cannot access without the aid and support
of, yes, doctors. We call this
phenomenon “information asymmetry,” and sufficient demand for doctors is all
the driving force necessary to incentivize a supply for them in the
marketplace. Vice-versa, a supply of
doctors in the marketplace will induce demand.
When tastes, preferences, and population are held constant, the only
true, measurable variables are the price paid for by patients, received by
doctors, based upon the quantity of services exchanged between them. Service quality may be an assumption by those
on the demand side, but aside from government- and industry-mandated
requirements, not much else enters into the equation.
So let us now return to
discuss this specific, real-life diabetic’s dilemma. There are two cases here: 1) you are not
prepared with any information, or 2) you have done your homework. Let’s take a look first at those that are not
prepared and, instead, will rely on their doctor to give the optimal treatment
with the intent on following it.
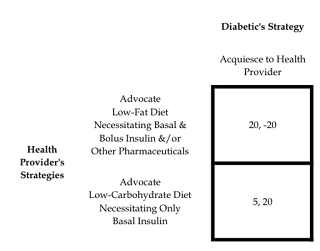
The above table shows the
asymmetrical relationship. Note that the
real power comes from the health-provider’s strategy, as they ultimately decide
which treatment the diabetic will follow, and, subsequently, the payoffs. Although the payoffs noted in the table are
assertions, those assertions are based upon the evidence presented in the
previous chapter. Recall that the first
number is the payoff for the row player, the health-provider, and the second
number is the payoff for the column player, the diabetic. The numbers themselves are somewhat
arbitrary, however, they are used here for illustrative purposes; namely, that
a low-fat diet, with corresponding necessity for a high consumption of
carbohydrates, will lead to an increase in free radicals and oxidative stress
in the body, and, if bolus insulin is taken, the risk of hypoglycemia is
ever-present. When the health-provider
recommends, and the diabetic follows, the low-fat diet, utilizing both basal
and bolus insulin, and perhaps other drugs too, the diabetic’s payoff is -20.
“Health-provider” is a
deliberately general title, as it may include all those influencers noted in
the previous chapter and more, including pharmaceutical companies, pharmacists,
researchers, doctors, endocrinologists, nutritionists, educators, the American
Diabetes Association, the World Health Organization, medical schools, nurses,
reference media such as the Physician’s Desk Reference, food manufacturers,
food marketers, popular internet sites, print media, the news, friends, family,
co-workers & acquaintances.
Moreover, the payoff at this
point for the diabetic is -20 because the diabetic now returns again and again
for checkups, providing a fee to the clinic each time; some of the stated
health-providers, doctors especially, are in the business of patient management. This system keeps the dutiful patient coming
back for regular doctor appointments, while at the same time keeping the
pharmacist busy refilling prescriptions.
And medical insurance coverage becomes an absolute necessity. Of course, the health-provider’s payoff is
+20, because they’re the ones being paid.
They espouse party-line mis-information due to the constraints of their
clinical practice guidelines; and, given the perceived information asymmetry,
most patients will believe them. The final irony is the report that physicians
frequently choose low-carbohydrate diets for themselves while recommending
low-fat for their patients.[17]
Now let’s imagine the case of
a symmetrical relationship between health-providers and diabetics. In the next table, we’ll enable the diabetic
with power of his/her own: the ability to make an informed choice regarding
their treatment, based upon the insight imparted by cited authors.
In PRISONER’S DILEMMA,
William Poundstone described how Dr. John Nash[18]
proved that every two-person finite game has at least one equilibrium point,
but that there are a few catches. These
equilibrium points can have “strange and undesirable properties.” In fact, sometimes Nash equilibriums appear
to be distinctly irrational.
The best solution for our
diabetic is to always “insist on a low-carbohydrate diet.” This strategy earns, on average, 20 “points,”
whereas, acquiescing to the health-provider earns, on average, zero. But contrast that to the health-provider’s
strategies. On average, they receive 5
“points” for doing the right thing, whereas, if they always preach party-line,
that is, advocate a low-fat diet with basal and bolus insulin, and perhaps
other drugs, they will earn on average 12.5 “points.”
Is that not a strange and undesirable
property? The client-health-provider
relationship is now on its head. The
payoff “incentivizes” all health-providers to advocate the deleterious diet
plus ample meds. We—the patients—are now
responsible for teaching and training them.
And we pay the health-providers for the opportunity to do so.
Whether or not they can be
trained is another matter entirely.
We’ve seen that it is in their best interest to always choose the
“advocate low-fat diet” strategy, and this is the diet based upon certain
standards of care. Those standards of
care, at least in North American and European societies, are called Clinical
Practice Guidelines (CPGs), and they are intended to present a synthesis of
current evidence and recommendations preformed by expert clinicians and may
affect the practice of large numbers of physicians. As a result, any influence that the authors
of CPGs experience from their interactions with pharmaceutical companies may be
transmitted many times over to the readers of CPGs. Consequently, if individual authors have
relationships that pose a potential conflict of interest, readers of these CPGs
may wish to know about them to evaluate the merit of those guidelines.
In
2002, Niteesh K. Choudhry, M.D., Henry
Thomas Stelfox, M.D., and Allan S. Detsky, M.D., Ph.D., surveyed authors of
CPGs throughout North America and Europe to find out the extent to which the
authors of CPGs interact with the pharmaceutical industry. They were seeking to provide empirical
evidence concerning this issue to improve the process of CPG development in the
future. Here are the conclusions from
that study:
“Eighty-seven
percent of authors had some form of interaction with the pharmaceutical
industry. Fifty-eight percent had
received financial support to perform research and 38% had served as employees
or consultants for a pharmaceutical company.
On average, CPG authors interacted with 10.5 different companies. Overall, an average of 81% (95% confidence
interval, 70%-92%) of authors per CPG had interactions. Similarly, all of the CPGs for 7 of the 10
diseases included in our study had at least 1 author who had some
interaction. Fifty-nine percent had
relationships with companies whose drugs were considered in the guideline they
authored, and of these authors, 96% had relationships that predated the
guideline creation process. Fifty-five
percent of respondents indicated that the guideline process with which they
were involved had no formal process for declaring these relationships. In published versions of the CPGs, specific
declarations regarding the personal financial interactions of individual
authors with the pharmaceutical industry were made in only 2 cases. Seven percent thought that their own
relationships with the pharmaceutical industry influenced the recommendations
and 19% thought that their coauthors’ recommendations were influenced by their
relationships.”[19]
Although
the survey’s response rate was low,[20]
there appears to be considerable interaction between CPG authors and the
pharmaceutical industry.
The most interesting, and perhaps regrettable, part of the discussion on
clinical practice guidelines, is that there isn’t one, universally accepted
guideline for diabetes. There is one
universally established way of looking at gravitation & gravity—gravitation
is a general term describing the phenomenon by which bodies with mass are
attracted to one another, while gravity refers specifically to the net force
exerted by the Earth on objects in its vicinity as well as by other factors,
such as the Earth’s rotation—but, like politics, there are many diabetes
treatment paradigms.
There are guidelines written for type 1 and 2 diabetes from the American
Association of Clinical Endocrinologists, the American Academy of Family
Physicians, the American Geriatrics Society, the Canadian Diabetes Association,
the Institute for Clinical Systems Improvement, the National Institute for
Health and Clinical Excellence, the Scottish Intercollegiate Guidelines
Network, and the Veterans Health Administration. In fact, each independent health-provider, or
health-providing group may have their own clinical practice guidelines. Utilizing GOOGLE for a quick internet search
of “Clinical Practice Guidelines Diabetes” returned 1,500,000 hits, where I
found the 2009 Clinical Practice Guidelines for Malaysia, which, by the way, and, of
course, encouraged a balanced diet consisting of 50-60% energy from
carbohydrate, 15-20% energy from protein and 25-30% energy from fats, not to
mention a high fibre diet.[21]
But one organization, the American Diabetes Association, provides the most
commonly cited and adopted guidelines in the US, and, perhaps, throughout the
world.
According to their website:
“The Association funds
research to prevent, cure and manage diabetes; delivers services to hundreds of
communities; provides objective and credible information; and gives voice to
those denied their rights because of diabetes.
Founded in 1940, our mission is to prevent and cure diabetes and to improve
the lives of all people affected by diabetes.”[22]
Quite a noble mission. In fact, they
do allocate millions of dollars per year toward research; in 2008, it was
approximately $43 million.[23] But our focus here is not the relative good
that they do in the world, for surely a person with type 1 diabetes that eats
carbohydrates and undergoes an intensive insulin regimen is far better off than
one that solely eats carbohydrates at will, given that their body’s cells lack
an effective glucose uptake mechanism.
Rather, it is the inherent conflict between the ADA’s conclusions
promulgated through guidelines, and who supports that platform, that is of
particular concern.
Cutting to the chase, the ADA works in its own best interest as evidenced
by the following, taken directly from their conflict of interest policy:
“The American Diabetes
Association and its subsidiaries (collectively, the Association) requires all
members of the Board of Directors, members of Board-appointed committees and
staff to act solely in the best interest of the Association without regard to
their personal or business interests.”[24]
The ADA isn’t as altruistic
as one would like to believe. They don’t
act primarily in the interest of diabetics; but, instead, in their own best
interest, and, at least in appearance, based upon their guidelines—as we will
shortly see—in the interest of their main stakeholders. But just who are their main
stakeholders? According to the ADA’s
strategic plan, the folks that have the deepest pockets from which the ADA will
base their growth upon are the corporate and pharmaceutical organizations, for
whom the following strategy applies:
“Maximize
corporate, pharmaceutical and foundation contributions to achieve revenue of
$42 million, which reflects an annual compound growth rate of 9.1%.”[25]
Nothing
at first can appear more difficult to believe than that the American Diabetes
Association, a credible, long-standing institution in the community, does not
necessarily act in the best interest of those most negatively affected by the
complications of diabetes. The truth of
the following assertion, however, cannot be disputed: the only way to get
pharmaceutical companies to contribute at that level, i.e., $42,000,000 per
year, and at that growth rate, i.e., 9.1%, is to serve their interests; the only
way to effect that is to directly or indirectly support the use of their
products, which, of course, are the many insulins and their compliments. And the only way to support that endeavor is
to espouse carbohydrates as an essential source of energy. A source of energy; yes, exogenous
carbohydrates are that. An essential
source of energy? No. Homo sapiens can manufacture their own glucose
in the liver after the ingestion and digestion of exogenous fat and protein.[26]
So
let’s now look a little more closely at the ADA’s Guidelines. I’ll call this story “The Tale of the Tell.”
As late as 2006 and 2007, the ADA’s position, promulgated sedulously
through their guidelines, was that “Low-carbohydrate diets (restricting total
carbohydrate to <130 g/day) are not recommended in the management of
diabetes,” and that “Saturated fat intake should be <7% of total calories.”[27] The ADA in 2006 wrote:
“Low-carbohydrate diets are not recommended in the management of
diabetes. Although dietary carbohydrate
is the major contributor to postprandial glucose concentration, it is an
important source of energy, water-soluble vitamins and minerals, and
fiber. Thus, in agreement with the
National Academy of Sciences-Food and Nutrition Board, a recommended range of
carbohydrate intake is 45–65% of total calories. In addition, because the brain and central
nervous system have an absolute requirement for glucose as an energy source,
restricting total carbohydrate to <130 g/day is not recommended.”[28]
They went on to state:
“Similar to the general population, people with diabetes are encouraged to
choose a variety of fiber-containing foods, such as legumes, fiber-rich cereals
(≥5 g fiber/serving), as well as fruits, vegetables, and whole-grain products
because they provide vitamins, minerals, fiber, and other substances important
for good health.”[29]
And, of course, the Guidelines were based upon
the DCCT:
“The DCCT clearly showed that intensive insulin therapy (three or more
injections per day of insulin or continuous subcutaneous insulin infusion
(CSII, or insulin pump therapy) was a key part of improved glycemia and better
outcomes. At the time of the study,
therapy was carried out with short- and intermediate-acting human insulins. Despite better microvascular outcomes, intensive
insulin therapy was associated with a marked increase in severe hypoglycemia
(62 episodes per 100 patient-years of therapy).
Since the time of the DCCT, a number of rapid-acting and long-acting
insulin analogs have been developed.
These analogs were designed to be more “physiological” in their
pharmacokinetics and pharmacodynamics and are associated with less hypoglycemia
with equal A1C lowering in type 1 diabetes.
Therefore, recommended therapy for type 1 diabetes consists of the
following components: 1) use of multiple dose insulin injections (3–4
injections per day of basal and prandial insulin) or CSII therapy; 2) matching
of prandial insulin to carbohydrate intake, premeal blood glucose, and
anticipated activity; and 3) for many patients (especially if hypoglycemia is a
problem), use of insulin analogs. There
are excellent reviews available that guide the initiation and management of
insulin therapy to achieve desired glycemic goals.”[30]
And in 2007, not much had changed:
“Low-carbohydrate diets (restricting total carbohydrate to <130 g/day)
are not recommended in the treatment of overweight/obesity [or in
diabetes]. The long-term effects of
these diets are unknown, and although such diets produce short-term weight
loss, maintenance of weight loss is similar to that from low-fat diets and the
impact on CVD risk profile is uncertain.”[31]
But then in 2008, what seems like a
sea-change occurred in the ADA’s Guidelines.
For the first time, the ADA added the following:
“For weight loss, either low-carbohydrate
or low-fat calorie-restricted diets may be effective in the short term (up to 1
year).”[32]
Though a subtle caveat was placed
on the low-carbohydrate diet:
“For patients on low-carbohydrate
diets, monitor lipid profiles, renal function, and protein intake (in those
with nephropathy), and adjust hypoglycemic therapy as needed.”[33]
And although I have been able to
find hundreds of studies concluding then espousing the efficacy of
low-carbohydrate diets, the ADA justified their position with only three:
“The optimal macronutrient
distribution of weight loss diets has not been established. Although low-fat diets have traditionally
been promoted for weight loss, several randomized controlled trials found that
subjects on low-carbohydrate diets (<130 g/day of carbohydrate) lost more
weight at 6 months than subjects on low-fat diets; however, at 1 year, the
difference in weight loss between the low-carbohydrate and low-fat diets was
not significant and weight loss was modest with both diets. Another study of overweight women randomized
to one of four diets showed significantly more weight loss at 12 months with
the Atkins low-carbohydrate diet than with higher-carbohydrate diets. Changes in serum triglyceride and HDL
cholesterol were more favorable with the low-carbohydrate diets. In one study, those subjects with type 2
diabetes demonstrated a greater decrease in A1C with a low-carbohydrate diet
than with a low-fat diet. A recent
meta-analysis showed that at 6 months, low-carbohydrate diets were associated
with greater improvements in triglyceride and HDL cholesterol concentrations
than low-fat diets; however, LDL cholesterol was significantly higher on the
low-carbohydrate diets.”[34]
Still, the ADA, in 2008, remained
firmly planted in making sure folks ingest their 130 grams of carbohydrates per
day:
“The recommended dietary allowance
(RDA) for digestible carbohydrate is 130 g/day and is based on providing
adequate glucose as the required fuel for the central nervous system without
reliance on glucose production from ingested protein or fat. Although brain fuel needs can be met on
lower-carbohydrate diets, long-term metabolic effects of very-low-carbohydrate
diets are unclear, and such diets eliminate many foods that are important
sources of energy, fiber, vitamins, and minerals and are important in dietary
palatability.”[35]
And the DCCT continued to be
cited as the holy grail:
“Glycemic control is fundamental to
the management of diabetes. The DCCT, a
prospective, randomized, controlled trial of intensive versus standard glycemic
control in type 1 diabetes, showed definitively that improved glycemic control
is associated with sustained decreased rates of microvascular (retinopathy and
nephropathy) as well as neuropathic complications. Follow up of the DCCT cohorts in the
Epidemiology of Diabetes Interventions and Complications (EDIC) study has shown
persistence of this effect in previously intensively treated subjects, even
though their glycemic control has been equivalent to that of previous standard
arm subjects during follow-up. In
addition, EDIC has shown a significant reduction of the rate of cardiovascular
outcomes in the previous intensive arm.
The DCCT clearly showed that
intensive insulin therapy (three or more injections per day of insulin or
continuous subcutaneous insulin infusion [CSII, or insulin pump therapy]) was a
key part of improved glycemia and better outcomes. At the time of the study, therapy was carried
out with short- and intermediate-acting human insulins. Despite better microvascular outcomes,
intensive insulin therapy was associated with a marked increase in severe
hypoglycemia (62 episodes per 100 patient-years of therapy). Since the time of the DCCT, a number of
rapid-acting and long-acting insulin analogs have been developed. These analogs were designed to be more
“physiological” in their pharmacokinetics and pharmacodynamics, and are
associated with less hypoglycemia with equal A1C lowering in type 1 diabetes.
Therefore, recommended therapy for
type 1 diabetes consists of the following components: 1) use of multiple dose
insulin injections (3–4 injections per day of basal and prandial insulin) or
CSII therapy; 2) matching of prandial insulin to carbohydrate intake, premeal
blood glucose, and anticipated activity; and 3) for many patients (especially
if hypoglycemia is a problem), use of insulin analogs. There are excellent reviews available that
guide the initiation and management of insulin therapy to achieve desired glycemic
goals.”[36]
The 2009 ADA Guidelines are replicated from those of 2008. The DCCT continues to serve as the foundation
of their Guidelines—the foundation to a house of cards—as it “clearly showed that intensive insulin therapy was a key part of improved
glycemia and better outcomes.” Yet I, and
countless others, who simply don’t eat many carbohydrates, and therefore
haven’t a need for an intensive insulin treatment, able to keep our glucose
levels within a normal range, simply, effectively, and efficiently, wonder not
who holds the extreme, unsupported view.
William Poundstone stated at
the end of his book that “The only satisfying solution to the prisoner’s
dilemma is to avoid prisoner’s dilemmas.”[37] Options in applying that to our situation are
rather limited. Clearly, not getting
diabetes is the ideal. Not sure how to
accomplish that with any level of confidence, so let’s move on to something a
little more promising. A vaccine—two
such vaccines in the works are GAD-alum and BCMA—might be a little late for
type 1s without any remaining beta function, but if they can save the beta
cells of anyone, then I’m all for it.[38]
One could simply live in a
state of denial, eating carbohydrates at will, not checking their BG, too, not
seeing any health providers. Yes, it is
a simple option, though, not very effective or efficient.
We’re really left with one
simple, inexpensive, non-time consuming, effective, efficient option. It is both the way to solve and the way to
avoid the prisoner’s dilemma. And we’ve
known about it, sans the basal insulin, for centuries.
[1] The statements “This book is written…” and “shall
continue to add footnotes…” and “I wrote this book…” are all from the first
paragraph of the Preface to Dawkins, Richard. The Blind Watchmaker: Why the Evidence of
Evolution Reveals a Universe Without Design.
New York: W.W. Norton & Company, page XV. Of course, he was referring to “our own
existence” and not an optimal solution to diabetes, however, the constructs fit
so well in this book’s context that I just had to use them.
[2] See Poundstone, William. Prisoner’s Dilemma; John Von Neumann, Game
Theory, and the Puzzle of the Bomb. New
York: Doubleday, 1992, pages 117-119.
[3] For a
particularly good discussion of Plato’s The Republic and the role of doctors,
see Terence Irwin’s Plato’s Ethics (Oxford University Press, 1995, pages
351-352). “Does Plato expect anything
more from people with wisdom than he would expect from them if they simply had
correct belief? In some striking and
important passages of the Laws, Plato makes it clear that he expects them to
display one distinguishing feature of knowledge in contrast to belief. They must understand why the things they are
told are right and good really are right and good; they must not simply take
other people’s word for it. To explain
this demand, Plato introduces a comparison with doctors. On the one hand, the slave doctor, who also gives
treatment to slaves, just gives instructions without giving any reason for
them. The free doctor, on the other
hand, who treats free people, explains why the treatment prescribed is the best
one for the patients. Instead of simply
giving orders, the free doctor discusses the patients’ conditions with them and
tells them enough to persuade them that the treatment being prescribed is the
best one for them (719e7-720e5 in The Republic). This discussion involves communicating some
theortetical understanding to the patient...”
[4] Stell, L Two cheers for physicians’ conflicts of
interest. Mt Sinai J Med 2004;71,236-242.
Available online at
http://www.ncbi.nlm.nih.gov/pubmed/15365589?dopt=Abstract. Retrieved on 3/14/09.
[5] McDowell, TJ Physician self referral arrangements:
legitimate business or unethical “entrepreneurialism.” Am J Law Med
1989;15,61-109. Available online at
http://www.ncbi.nlm.nih.gov/pubmed/2764015?dopt=Abstract. Retrieved on 3/14/09.
[6] Moore, N Entrepreneurial doctors and lawyers: regulating
business activity in the medical and legal professions. Spece, R Shimm, D
Buchanan, A eds. Conflicts of interest in clinical practice and research
1996,171-196, New York, NY: Oxford University Press.
[7] Kouri, B, Parsons, R, Alpert, H Physician self-referral
for diagnostic imaging: review of the empiric literature. AJR Am J Roentgenol
2002;179,843-850. Available online at http://www.ajronline.org/cgi/content/full/179/4/843?ijkey=9700ac1ab1459c8a27e2b9a0084d5137b80d8ec2&keytype2=tf_ipsecsha. Retrieved on 3/14/09. See also Mitchell, J, Sass, T Physician
ownership of ancillary services: indirect demand inducement or quality
assurance? J Health Econ 1995;14,263-289.
Available online at http://www.ncbi.nlm.nih.gov/pubmed/10145136?dopt=Abstract. Retrieved on 3/14/09. See also Nallamothu, B, Rogers, M, Chernew,
M, et al Opening of specialty cardiac hospitals and use of coronary
revascularization in Medicare beneficiaries. JAMA 2007;297,962-968. Available online at http://jama.ama-assn.org/cgi/content/abstract/297/9/962?ijkey=bfc824f70f476933c2c4d63f1fa858999211ce44&keytype2=tf_ipsecsha. Retrieved on 3/14/09.
[8] See Tonelli, M.D., M.A., FCCP, Mark R. “Conflict of Interest in Clinical Practice,” Chest
August, 2007, vol. 132, no. 2, 664-670.
doi: 10.1378/chest.07-0315.
Available online at
http://www.chestjournal.org/content/132/2/664.full#ref-21. Retrieved on 3/14/09.
[9] Angell, M The
Truth About Drug Companies. 2004 Random House. New York, NY. See also Kassirer, J On the Take: How
Medicine’s Complicity with Big Business Can Endanger Your Health. 2004 Oxford
University Press. New York, NY. See also
Blumenthal, D Doctors and drug companies. N Engl J Med 2004;351,1885-1890. Available online at
http://content.nejm.org/cgi/content/full/351/18/1885?ijkey=0423b68ab05b7d39ec9e9bbd72d1f905e82f10da&keytype2=tf_ipsecsha. Retrieved on 3/14/09. “Interactions
between drug companies and doctors are pervasive. Relationships begin in medical school,
continue during residency training, and persist throughout physicians’
careers. The pervasiveness of these
interactions results in part from a huge investment by the pharmaceutical
industry in marketing. In 2002, the
industry expended 33 percent of its revenues on "selling and
administration.” In 2001, one company,
Novartis, reported spending 36 percent of its revenues on marketing alone. The marketing expenditures of the drug
industry have been estimated variously at $12 billion to $15 billion yearly, or
$8,000 to $15,000 per physician. In
2001, the industry's sales force of drug detailers, whose job is to meet
individually with physicians and promote company products, numbered nearly
90,000 in the United States—1 salesperson for every 4.7 office-based
physicians.”
[10] Kassirer,
J. On the Take: How Medicine’s
Complicity with Big Business Can Endanger Your Health. New York: Oxford University Press, 2004.
[11] Moynihan, R Who pays for the pizza? Redefining the
relationships between doctors and drug companies: 1. Entanglement. BMJ
2003;326,1189-1192. Available online at
http://www.bmj.com/cgi/content/full/326/7400/1189?ijkey=1d0ba84bbe6c5e26d9cc59d1ab5e10bef47b6921&keytype2=tf_ipsecsha. Retrieved on 3/14/09.
[12] See Tonelli, M.D., M.A., FCCP, Mark R. “Conflict of Interest in Clinical Practice,” Chest
August, 2007, vol. 132, no. 2, 664-670.
doi: 10.1378/chest.07-0315.
Available online at
http://www.chestjournal.org/content/132/2/664.full#ref-21. Retrieved on 3/14/09.
[13] See “A National Survey of Physician-Industry
Relationship,” Campbell EG, Gruen RL, Mountford J, Miller LG, Cleary PD,
Blumenthal D. N Engl J Med. 2007 Apr
26;356(17):1742-50. Available online at
http://content.nejm.org/cgi/content/full/356/17/1742. Retrieved on 3/14/09.
[14] See “Why do Doctors Use Treatments That Don't Work?” online at http://articles.mercola.com/sites/articles/archive/2004/03/13/doctor-treatments.aspx. Retrieved on 4/18/08. There are many more articles available on Dr.
Mercola’s website on point. See, for
example, “Medical Research or Drug Company Secrets?” online at http://articles.mercola.com/sites/articles/archive/2002/11/20/drug-companies-part-nine.aspx;
“The Doors Of Perception: Why Americans Will Believe Almost Anything,” at http://articles.mercola.com/sites/articles/archive/2001/08/15/perception.aspx;
“Drugs and Doctors May be the Leading Cause of Death in U.S.” at http://articles.mercola.com/sites/articles/archive/2003/01/15/doctors-drugs-part-two.aspx;
“Doctors Are The Third Leading Cause of Death in the US, Causing 250,000 Deaths
Every Year,” at http://articles.mercola.com/sites/articles/archive/2000/07/30/doctors-death-part-one.aspx;
“Why Doctors Are 9,000 Times More Likely to Accidentally Kill You Than Gun
Owners,” at http://articles.mercola.com/sites/articles/archive/2000/05/14/doctor-accidents.aspx;
and “Shame: A Major Reason Why Most Medical Doctors Don't Change Their Views,” at http://articles.mercola.com/sites/articles/archive/2002/03/30/doctors-shame.aspx. All online articles retrieved on 4/18/09.
[15] See Groves, Barry.
Trick and Treat: How ‘Healthy Eating’ is Making us Ill. London, UK: Hammersmith Press Limited, 2008,
pages 30-31. Used by permission
[16] For a compeling discussion from the point of view of
a practicing medical doctor and ethicist, see Lantos, John D. Do We Still Need Doctors: A Physician’s
Personal Account of Practicing Medicine Today.
New York: Routledge, 1997.
[17] See La Puma J, Szapary P, Maki KC. Physicians
recommendations for and personal use of low-fat and low-carbohydrate diets. Int J
Obes Relat Metab Disord. 2005;29:251–253.
doi: 10.1038/sj.ijo.0802840. Available
online at http://www.ncbi.nlm.nih.gov/pubmed/15534615. Retrieved on 7/29/09.
I am grateful to the
authors Surender K Arora and Samy I McFarlane, as the quote comes from their article entitled: “The Case for Low Carbohydrate Diets in
Diabetes Management,” Nutr Metab (Lond). 2005; 2: 16. Published online 2005 July 14. doi:
10.1186/1743-7075-2-16. PMCID: PMC1188071. Available online at
http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=1188071. Retrieved on 7/29/09.
[18] The subject of the film A Beautiful Mind was John
Forbes Nash, Jr. Dr. Nash did not have
diabetes, but he was the most notable of the schizophrenic patients treated in
the Insulin Coma Unit at Trenton Psychiatric Hospital (TPH) in West Trenton,
New Jersey, in 1961. An American mathematician
and economist whose works in game theory, differential geometry, and partial
differential equations provided insight into the forces that govern chance and
events inside complex systems in daily life, his theories are still used today
in market economics, computing, accounting and military theory. Serving as a Senior Research Mathematician at
Princeton University during the later part of his life, he shared the 1994
Nobel Memorial Prize in Economic Sciences with game theorists Reinhard Selten
and John Harsanyi.
In 1961, John was committed by Alicia and his
sisters to Trenton State Hospital in New Jersey. There, he was subjected to insulin-coma
therapy, which involved injecting the patient with large amounts of insulin to
put them into a coma, often causing seizures.
His colleagues in mathematics were outraged and wrote a letter to the
hospital, urging the doctors to protect his mind for the good of humanity. He was discharged after six months of the
insulin treatment and looked absolutely terrible to his family members.
Dr. Manfred Sakel, a Viennese
psychiatrist, developed the technique of Insulin Coma Therapy (ICT) in 1928 and
introduced it to the United States in 1936.
Nondiabetic patients with schizophrenia and major depression were
treated with ICT 5 days a week for 6 weeks.
The insulin unit at TPH
treated 24 males and 24 females daily in separate wards. The initial dose of regular insulin was 10–20
units administered intramuscularly at 7:00 a.m. in the unit; the dose was
increased by about 10 units per day to about 90–100 units until hypoglycemic
coma developed. A team of trained nurses
and physicians supervised the care of the patients, who rested on litters. In some patients, more than 100 units of
insulin were needed to produce coma.
After 30–60 minutes of
hypoglycemic coma, nurses reversed the condition by intragastric glucose
solution or Karo syrup. Patients were
carefully observed until cognitive, returned to their room, and then provided
meals and snacks.
In her book A Beautiful Mind,
Sylvia Nasar reports that Dr. Nash first showed the overt signs of
schizophrenia in 1959 when he began to see encrypted messages in newspaper
stories. He was teaching at the
Massachusetts Institute of Technology and after a poorly presented lecture in
March, he was involuntarily committed to the McLean Hospital, a private
hospital for wealthy patients affiliated with the Harvard Medical School in
Boston.
He received injections of
chlorpromazine but the principal treatments offered were psychotherapy, group
therapy, and counseling. After a stay of
50 days, he was released. In May, his wife
gave birth to a son. He was not able to
return to work, and for the next two years, in the grip of a persistent
psychosis, he roamed Europe.
He underwent 6 weeks of
insulin coma treatment. When he was
released from the hospital, he was much improved. His thoughts were under control and he was
able to once again work on a scientific paper.
From July of 1961 to August 1962, he worked at Princeton.
His illness recurred and
sadly, further treatment was refused. He
spent the next decades as a shadowy figure on the Princeton University campus.
Why
was Dr. Nash treated with ICT? In 1961, the options available for patients
with schizophrenia were antipsychotic drugs, Electroconvulsive Therapy (ECT),
insulin coma, and lobotomy. The optimal
treatment was believed to be chlorpromazine, although many psychiatrists still
looked to ECT for its benefits. When
chlorpromazine failed, ECT was the realistic option. While most psychiatric hospitals had
abandoned ICT, it had persisted at Trenton State Hospital, and it was a logical
offering when these other treatments were refused. (Lobotomy was no longer a
realistic option, having been replaced by antipsychotic drugs.)
For biographical information
see the Wikipedia article entitled “John Forbes Nash, Jr.” online at
http://en.wikipedia.org/wiki/John_Forbes_Nash; see also
http://nobelprize.org/nobel_prizes/economics/laureates/1994/nash-autobio.html. Both retrieved on 3/14/09. See also
http://www.pbs.org/wgbh/amex/nash/filmmore/ps_ict.html. Retrieved on 3/1/09.
For information about IST,
see Sakel M: The Pharmacological Shock Treatment of Schizophrenia. New York,
Nervous and Mental Diseases Publishing Co., 1938. See also Sakel M: The Insulin Treatment of
Schizophrenia. In An Introduction to
Physical Methods of Treatment in Psychiatry. 1st edition. Sargent W, Slater E,
Eds. Edinburgh, U.K., E. & S. Livingstone, 1944. See also Fink, M., Shaw, R., Gross, G., and
F. S. Coleman. “Comparative study of chlorpromazine and insulin coma in the
therapy of psychosis.” Journal of the American Medical Association. 1958;
166:1846-50. See also Rinkel, M., and H.
E. Himwich. Insulin Treatment in Psychiatry. New York: Philosophical Library,
1959.
See
also Arthur Krosnick, MD, FACP, CDE, “Five Decades of Diabetes Patient Care:
The Time of My Life,” Clinical Diabetes
20:173-178, 2002.
And see Nasar
S. A Beautiful Mind. New York: Simon & Schuster, 1961, pages
288-294.
[19] See
“Guidelines and the Pharmaceutical Industry Relationships Between Authors of
Clinical Practice,” by Niteesh K. Choudhry, Henry Thomas Stelfox, and
Allan S. Detsky. JAMA.
2002;287(5):612-617; doi: 10.1001/jama.287.5.612. Available online at http://jama.ama-assn.org/cgi/reprint/287/5/612.pdf. Retrieved on
6/13/09.
[20] “One hundred twenty CPGs were identified by our search
strategy, of which 35 were excluded because a major North American or European
society did not endorse the CPG and 38 were excluded because they were
editorials about CPGs or comparisons of different CPGs. Therefore, 47 CPGs were initially
included. Subsequently, 1 CPG was
excluded because the authors could not be identified and 2 CPGs were excluded
after the authors had been surveyed since these were evaluations of CPGs rather
than actual CPGs. Therefore, 44 CPGs
with 192 authors were included in the study.
Current addresses of 13 authors could not be located and 3
authors had died, resulting in a total of 176 potentially contactable
authors. Of these, 107 authors (61%)
responded representing 37 of the 44 CPGs included in our study. Therefore, 7 guidelines were not represented
in our final sample. Despite this, all
of the disease states that were initially included in our study protocol were
still represented by at least 2 CPGs, with the exception of depression, for
which there was only 1 CPG included in the sample and for which we received a
response. Seven respondents refused to
participate, all of whom were involved with different guidelines. Three of these 7 authors were from Europe, 2
were from the United States, and 2 were from Canada. This left 100 completed surveys, which form
the basis of our results. Overall, the
response rate was 57% of potentially contactable authors and 52% of all authors
initially included in our sample. The
distribution of sex and disease to which the guidelines pertained was similar
for respondents and nonrespondents; however, the distribution of current
country of residence was not.
Sixty-three percent of authors currently residing in the United States
did not respond whereas 29% of authors living in Canada did not respond (P=.001). Twenty-eight (26%) of 107 authors responded
with a letter attached to their survey.
These letters could be interpreted as being supportive (21%), neutral
(57%), or critical (21%) of our study.
Of the 100 authors who completed the first survey, 1 had died and 1 had
moved and was unreachable, leaving 98 potentially contactable authors for the
second survey. Of these, 82 (83%)
responded. One of these authors refused
to participate and 1 could not recall the nature of the disclosure process and,
therefore, left the survey blank.
Consequently, the response rate for the second survey was 82%.” See Ibid.
[21] See “Clinical Practice Guidelines. Management of Type 2 Diabetes Mellitus (4th
Edition),” May, 2009. Malaysian
Endocrine & Metabolic Society, Ministry of Health Malaysia, Academy of
Medicine Malaysia, and Persatuan Diabetes Malaysia. Available online at
http://www.diabetes.org.my/article.php?aid=590.
Retrieved on 7/27/09.
[22] Available online at
http://www.diabetes.org/aboutus.jsp?WTLPromo=HEADER_aboutus&vms=302103524165. Retrieved on 7/28/09.
[23] See the ADA 2008 Consolidated Financials online at http://www.diabetes.org/uedocuments/2008_ADA_ConsolidatedFinancialsFS_Final.pdf. Retrieved on 7/38/09.
[24] See the American Diabetes Association “About Us” page
online at
http://www.diabetes.org/aboutus.jsp?WTLPromo=HEADER_aboutus&vms=302103523106. Retrieved on 7/28/09.
[25] American Diabetes Association
2008-2011 Strategic Plan. Available
online at
http://www.diabetes.org/uedocuments/2008-2011ADAStrategicPlan.pdf. Retrieved on 7/28/09.
[26] What limits the liver’s capacity to convert amino
acids to glucose? “Conversion of amino
acids to glucose involves several metabolic processes; deamination or
transamination, conversion of the released NH4+ to urea and finally synthesis
of glucose from amino acid residues. The
key to understanding the physiological limitation of glucose formation from
amino acids lies in the large amount of energy required to fuel these
processes. Energy in the sense used here
means the hydrolysis of adenosinetriphosphate (ATP) to either AMP + PPi or ADP
+ Pi. Four ATP molecules are used to
convert two NH4+ to urea and six more are required to convert the carbon
skeletons of these amino acids to glucose.
One ATP is also required to add a glucosyl group to a glycogen molecule
so, you see, a lot of energy is used in this process. All cells and tissues are built up such that
ATP levels are relatively stable. This
is a basic prerequisite for life. Under
gluconeogenesis the liver must rely upon aerobic metabolism to replace the ATP
that is consumed. By definition this is
an oxygen-dependent process. The “catch”
is that the liver obtains most of its oxygen from the portal vein where the
partial pressure of oxygen is rather low.
This limits uptake of oxygen, limits ATP production and, therefore, the
synthesis of glucose from amino acids. We have data about the total amount of oxygen
supplied to the human liver.
Calculations based on this (and assuming that all of this oxygen goes to
support conversion of amino acids to glucose) suggest that the maximum capacity
of hepatic glucose synthesis from amino acids lies around 400 grams/day. This is the equivalent of approximately 1600
kcal...” See “Rabbit
Starvation: High Protein and High Fat Diets,” by Professor Emeritus Robert S.
Horn. Available online at
http://www.medbio.info/Horn/PDF%20files/rabbit%20starvation.pdf. Retrieved on 12/16.09.
[27] See “Standards of Medical Care in Diabetes—2006,” Diabetes Care, January,
2006, vol. 29, no. suppl 1 s4-s42. Available online at
http://care.diabetesjournals.org/content/29/suppl_1/s4.full. Retrieved on 7/27/09.
[28] Ibid.
[29] Ibid.
[30] Ibid.
[31] See “Standards of Medical Care in Diabetes—2007,”doi:
10.2337/dc07-S004. Diabetes Care, January, 2007, vol. 30, no. suppl 1 S4-S41.
Available online at http://care.diabetesjournals.org/content/30/suppl_1/S4.full. Retrieved on 7/28/09.
[32] See “Standards of Medical Care in
Diabetes—2008,” doi:
10.2337/dc08-S012. Diabetes Care, January, 2008, vol. 31, no.
Supplement 1 S12-S54. Available online at http://care.diabetesjournals.org/content/31/Supplement_1/S12.full. Retrieved on 7/28/09.
[33] Ibid.
[34] Ibid.
[35] Ibid.
[36] Ibid.
[37] Poundstone, William.
Prisoner’s Dilemma: John Von Neumann, Game Theory, and the Puzzle of the
Bomb. New York: Doubleday, 1992, page 278.
[38] See “GAD Treatment and Insulin Secretion in
Recent-Onset Type 1 Diabetes,” by Johnny Ludvigsson, M.D., Ph.D., Maria
Faresjö, Ph.D., Maria Hjorth, M.Sc., Stina Axelsson, M.Sc., Mikael Chéramy,
M.Sc., Mikael Pihl, M.Sc., Outi Vaarala, M.D., Ph.D., Gun Forsander, M.D.,
Ph.D., Sten Ivarsson, M.D., Ph.D., Calle Johansson, M.D., Agne Lindh, M.D.,
Nils-Östen Nilsson, M.D., Jan Åman, M.D., Ph.D., Eva Örtqvist, M.D., Ph.D.,
Peter Zerhouni, M.Sc., and Rosaura Casas, Ph.D.
The New England Journal of
Medicine, Volume 359:1909-1920, October 30, 2008, Number 18. Available online at
http://content.nejm.org/cgi/content/full/359/18/1909. Retrieved on 5/30/09. See also http://www.dvdc.org.au/. Retrieved on 5/30/09. See also http://www.jdrf.org.au/news/view/research-breakthrough-type-1-diabetes-vaccine-a-step-closer. Retrieved on 5/30/09.